Knowing HRD status is important to determine advanced ovarian cancer treatment options
Homologous recombination deficiency (HRD) is present in approximately 48% of ovarian cancer tumors,1 most often resulting from a mutation found only within the tumor. Some causes of HRD are well established, while others remain unknown.2,3,4
Determining HRD status for ovarian cancer patients can help provide information on the magnitude of benefit for targeted therapies.
There are limitations to determining HRD status when evaluating each cause individually
HRD resulting from epigenetic events such as BRCA1 promoter methylation will be missed with a gene sequencing approach.5,6
HR pathway gene mutations other than BRCA1 and BRCA2 are rare, and it is unclear if they are connected to HRD.7,8
There is a distinct genomic effect associated with HRD.3
Evaluating LOH, TAI and LST allows for the assessment of HRD regardless of the specific cause.3
MyChoice CDx determines HRD status in multiple ways for comprehensive results
MyChoice CDx examines ovarian cancer tumors using two methods (BRCA1/2 mutation and genomic instability) to determine a patient’s HRD status.
BRCA1 & BRCA2 status
Sequence variants + Large rearrangements
- Detection and classification of sequence variants and large rearrangements
- Identification of somatic and germline variants present in the tumor
Genomic instability status
LOH + TAI + LST
- Comprehensive assessment of loss of heterozygosity (LOH), telomeric allelic imbalance (TAI) and large-scale state transitions (LST) across the entire genome
Not all HRD tests are alike
MyChoice CDx is recommended by ASCO
Myriad MyChoice CDx is the only commercial companion diagnostic included in the new recommendations from The American Society of Clinical Oncology (ASCO) for the treatment and management of certain patients with advanced ovarian cancer.
| MyChoice® CDx | |
|---|---|
| Landmark published clinical trials | PAOLA, PRIMA, SOLO1 |
| Guidelines | ASCO (by name), National Comprehensive Cancer Network |
| FDA-approval | Yes |
| HRD markers | tBRCA, LOH, TAI, LST |
| Comprehensive BRCA1/2 large rearrangements performed? |
Yes |
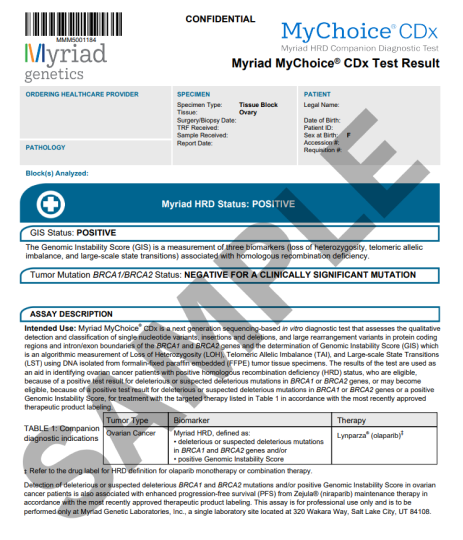
Clear, comprehensive results
To guide your ovarian cancer treatment decisions
Key report elements
- Genomic instability score (GIS) status
- Tumor mutation BRCA1/BRCA2 status (tBRCA1/2 status)
- Interpretation of any somatic BRCA1 and BRCA2 variants identified
- Overall test interpretation most relevant to patient management (if multiple variants detected)

How to test with Sponsored Testing Program for Myriad MyChoice CDx
MyChoice CDx typically delivers results in 14 days or less upon receipt of the sample
Provider completes the test request form
Provider completes the test request form
Myriad Genetics receives the TRF and sends a tumor specimen collection kit to the pathology lab
Myriad Genetics receives the TRF and sends a tumor specimen collection kit to the pathology lab
Tumor sample† arrives at Myriad Genetics lab and MyChoice CDx testing is performed
Tumor sample† arrives at Myriad Genetics lab and MyChoice CDx testing is performed
Results are sent to the ordering provider in the mail
Results are sent to the ordering provider in the mail
Tumor block is returned to the pathology lab immediately after result reporting
(slides will not be returned)
Tumor block is returned to the pathology lab immediately after result reporting
(slides will not be returned)
†MyChoice CDx is run on formalin-fixed paraffin-embedded (FFPE) ovarian tumor tissue

MyChoice resources
For questions regarding the MyChoice CDx Sponsored Testing Program, please call (877) 283-6709.
Sponsored Testing Program for Myriad MyChoice® CDx Terms and Conditions
The Myriad MyChoice CDx Sponsored Testing Program (the “Program”) is offered by AstraZeneca Pharmaceuticals (AstraZeneca) in order to address patient barriers to clinically appropriate, provider-prescribed testing. Through the Program, AstraZeneca, through an arrangement with Myriad Genetics (Myriad), makes the MyChoice CDx test available at no-charge for certain eligible patients with advanced ovarian cancer.
Patients must meet all of the following criteria to be eligible for the Program (collectively, the “Eligibility Criteria”):
- The patient has histologically confirmed advanced ovarian cancer
- The patient has received a prior test report that either:
- Has a tumor BRCA1/2 wild-type result from single gene test or multigene NGS panel (other than MyChoice CDx) or
- Has a germline BRCA1/2 wild-type result from a germline panel (collectively, a “Prior Test”)
- Myriad is able to use a previously collected tissue sample from the patient in order to complete the test
- Testing the patient’s sample is consistent with the MyChoice CDx label
- The patient has not previously received a MyChoice CDx test
The Program covers the cost of one MyChoice CDx test per eligible patient. To participate in the Program, the provider must submit to Myriad an attestation that confirms that: (i) the patient satisfies the Program Eligibility Criteria; (ii) the provider believes that the MyChoice CDx test is clinically appropriate and medically necessary for the patient; (iii) the provider is not seeking reimbursement for the MyChoice CDx test or other services provided in connection with the MyChoice CDx test; and (iv) the provider has obtained consent necessary to comply with applicable law.
The Program is open to any patient who meets the Eligibility Criteria, regardless of insurance status. There is no obligation to recommend, purchase, order, prescribe, promote, administer, use, or support any AstraZeneca, Myriad, or other third party product or service to participate in the Program.
The Program does not cover any additional services associated with the patient’s treatment, including the cost of tissue collection. No patient, provider, or payer, including government payers, are billed for the Program. Providers may not seek reimbursement from any patient or third party payer (including commercial health plans and government health care programs) for the MyChoice CDx test or other services provided in connection with the Program.
AstraZeneca does not receive patient- or provider-identifiable information in connection with the Program.
AstraZeneca retains the right to amend or rescind the Program at any time. While AstraZeneca provides financial support for the Program, tests and services are performed by Myriad. AstraZeneca assumes no liability and provides no warranties for the testing services provided by Myriad.
The Program is available only in the United States in the 50 states and District of Columbia.

-
MyChoice® CDx intended use
Myriad MyChoice® CDx is a next generation sequencing-based in vitro diagnostic test that assesses the qualitative detection and classification of single nucleotide variants, insertions and deletions, and large rearrangement variants in protein coding regions and intron/exon boundaries of the BRCA1 and BRCA2 genes and the determination of Genomic Instability Score (GIS), which is an algorithmic measurement of Loss of Heterozygosity (LOH), Telomeric Allelic Imbalance (TAI), and Large-scale State Transitions (LST) using DNA isolated from formalin-fixed paraffin embedded (FFPE) tumor tissue specimens.
The results of the test are used as an aid in identifying ovarian cancer patients with positive homologous recombination deficiency (HRD) status, who are eligible, because of a positive test result for deleterious or suspected deleterious mutations in BRCA1 or BRCA2 genes, or may become eligible, because of a positive test result for deleterious or suspected deleterious mutations in BRCA1 or BRCA2 genes or a positive Genomic Instability Score, for treatment with the targeted therapy listed in Table 1 in accordance with the most recently approved therapeutic product labeling.
Table 1: Companion diagnostic indicationsTumor Type Biomarker Therapy Ovarian Cancer Myriad HRD, defined as: - deleterious or suspected deleterious mutations in BRCA1 and BRCA2 genes and/or
- positive Genomic Instability Score
LYNPARZA® (olaparib)* * Refer to the drug label for HRD definition for olaparib monotherapy or combination therapy.
Detection of deleterious or suspected deleterious BRCA1 and BRCA2 mutations and/or positive Genomic Instability Score in ovarian cancer patients is also associated with enhanced progression-free survival (PFS) from Zejula® (niraparib) maintenance therapy in accordance with the most recently approved therapeutic product labeling. This assay is for professional use only and is to be performed only at Myriad Genetic Laboratories, Inc., a single laboratory site located at 320 Wakara Way, Salt Lake City, Utah 84108.
LYNPARZA is a registered trademark of the AstraZeneca group of companies.
US-81242 Last Updated 10/23
US-79743 Last Updated 9/23
References:
- Moore KN, Secord AA, Geller MA, et al. Niraparib monotherapy for late-line treatment of ovarian cancer (QUADRA): a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2019;20(5):636-648. doi:10.1016/S1470-2045(19)30029-4
- da Cunha Colombo Bonadio RR, Fogace RN, Miranda VC, Diz MDPE. Homologous recombination deficiency in ovarian cancer: a review of its epidemiology and management. Clinics (Sao Paulo). 2018;73(suppl 1):e450s. doi:10.6061/clinics/2018/e450s
- Watkins JA, Irshad S, Grigoriadis A, Tutt ANJ. Genomic scars as biomarkers of homologous recombination deficiency and drug response in breast and ovarian cancers. Breast Cancer Res. 2014;16(3):211. doi:10.1186/bcr3670
- Konstantinopoulos PA, Ceccaldi R, Shapiro GI, D’Andrea AD. Homologous recombination deficiency: exploiting the fundamental vulnerability of ovarian cancer. Cancer Discov. 2015;5(11):1137-1154. doi:10.1158/2159-8290.CD-15-0714
- Timms KM, Mills G, Perry M, Gutin A, Lanchbury J, Brown R. Comparison of genomic instability test scores used for predicting PARP activity in ovarian cancer. J Clin Oncol. 2020;38(suppl 15):1586. doi:10.1200/jco.2020.38.15_suppl.1586
- Baldwin RL, Nemeth E, Tran H, et al. BRCA1 promoter region hypermethylation in ovarian carcinoma: a population-based study. Cancer Res. 2000;60(19):5329-5333.
- Norquist BM, Harrell MI, Brady MF, et al. Inherited mutations in women with ovarian carcinoma. JAMA Oncol. 2016;2(4):482-490. doi:10.1001/jamaoncol.2015.5495
- Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474(7353):609-615. doi:10.1038/nature10166